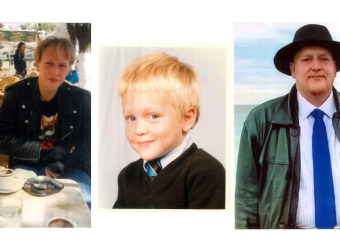
David’s battle with one of Britain’s biggest brain tumours
"They told me I might not survive, but here I am."
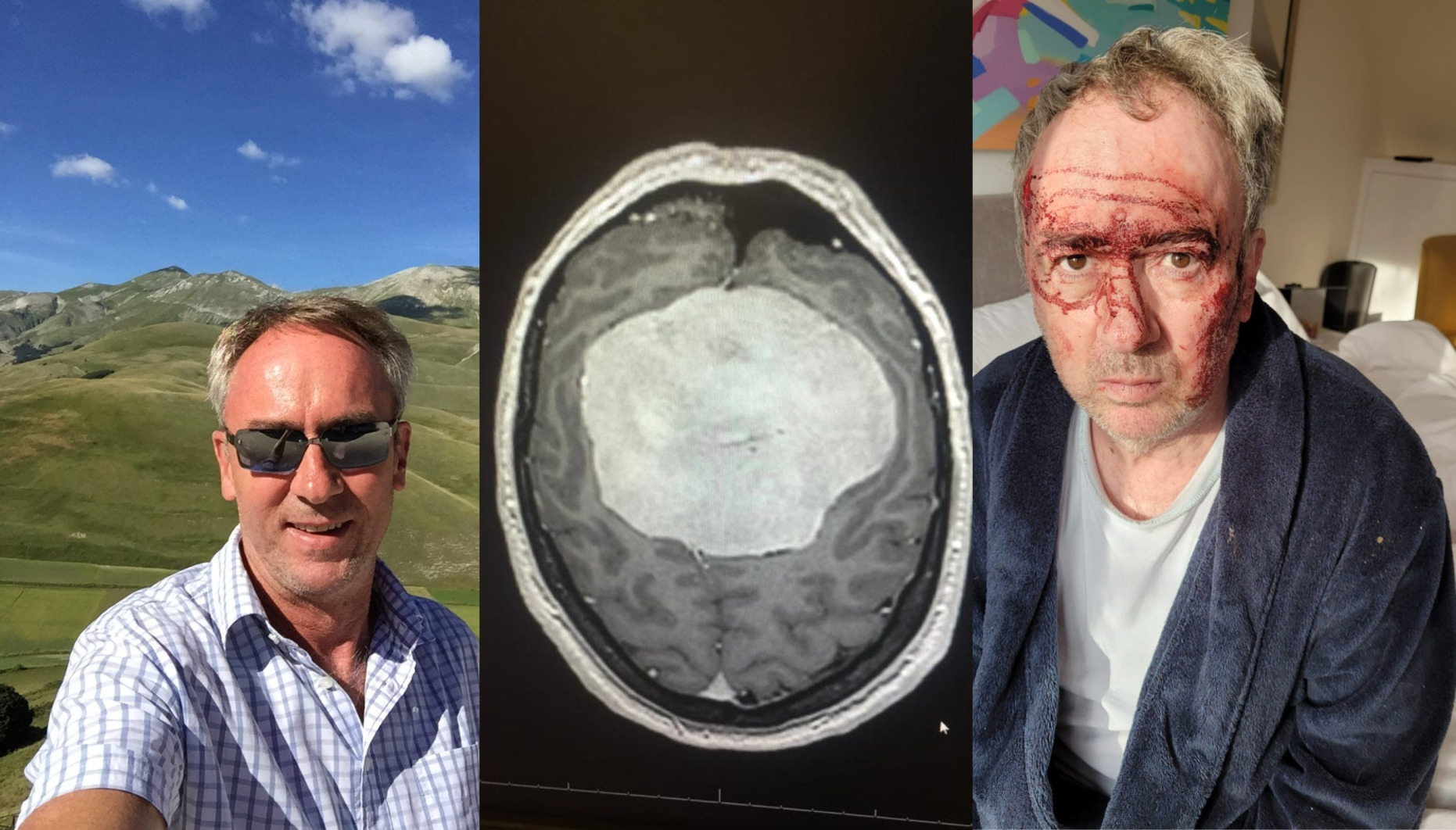
After a combined 28-hours of operations and several bleeds on the brain, David Baugh survived one of the largest brain tumours his doctors had ever seen in 2019. The tumour, diagnosed after a seizure, was only the first step of a long journey of recovery.
Brain tumours affect thousands of people every year in the UK, often arriving with no warning and life-altering consequences. One of those people is David Baugh, who had a long and successful career in the corporate world before his life was unexpectedly turned upside down.
In this guest blog, David, 59, shares how a seizure in late 2019 revealed something far more serious — and how recovery, setbacks, and resilience have shaped the next chapter of his life.
How it all started
David recalls:
“There were warning signs, but everybody missed them.”
David’s story began at the end of 2019 when his then-girlfriend witnessed him having a seizure. What followed was a series of hospital visits, starting with a shocking awakening:
“I remember waking up with this big ambulance chap at the end of the bed saying, ‘We’ll take you to hospital.’ I told him I’d drive myself. He said, ‘No, I insist, sir.'”
At Kingston Hospital, an MRI revealed something alarming: meningioma, a type of brain tumour.
“It turned out to be the one largest tumour anyone at St George’s Hospital had ever seen. Roughly the size of a grapefruit.”
What is a meningioma?
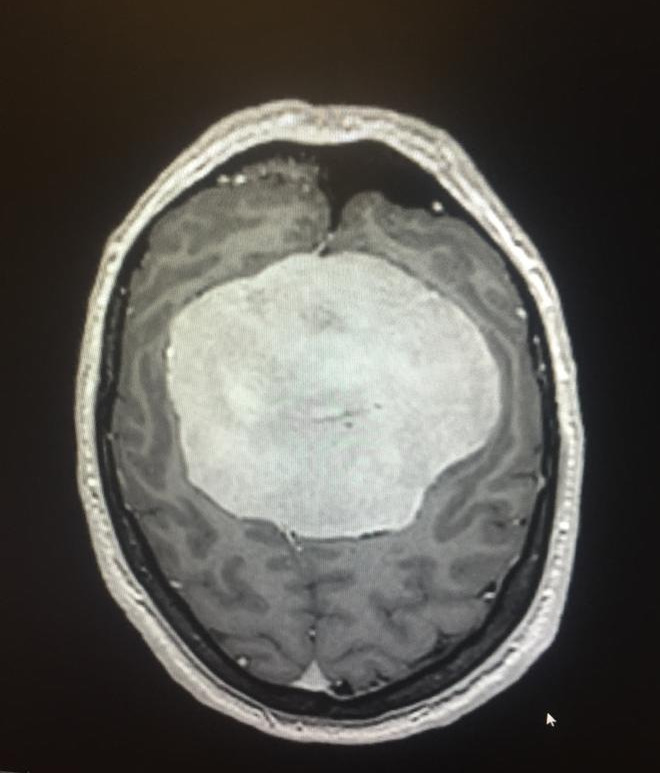
A meningioma is a type of brain tumour that forms in the meninges, the thin layers of tissue covering the brain and spinal cord. Most meningiomas are benign, meaning they are not cancerous and tend to grow slowly.
However, because they develop in the confined space of the skull, even non-cancerous tumours can cause significant symptoms by pressing on the brain or nearby nerves. Common signs include headaches, seizures, changes in vision, and memory issues, depending on the tumour’s size and location. Meningiomas are one of the most common types of brain tumours and are more frequently diagnosed in older adults and women.
Life-or-death decisions
Referred to St George’s Hospital in London, David was presented with two options by his surgeon, Dr Singh:
“Option one — we open your skull, take the tumour out, and you recover.
Option two — we leave it, and you might be dead in a few weeks.”
David chose the first option without hesitation.
He said:
“They told me I might not survive – but here I am.”
In 2020, he underwent a 21-hour craniotomy. The surgery was intense, followed by two bleeds on the brain, a second length of surgery and five months in the hospital, most of it in intensive care. His recovery took place during the height of the COVID-19 pandemic.
What is a craniotomy?

A craniotomy is a surgical procedure in which a portion of the skull is temporarily removed to allow surgeons to access the brain. It is commonly performed to remove brain tumours, relieve pressure, or treat conditions like aneurysms or traumatic brain injuries.
The procedure involves carefully cutting through the scalp, creating an opening in the skull, and gently working around delicate brain tissue to reach the affected area. Once the issue is treated — such as a tumour being removed — the bone flap is replaced and secured.
Recovery from a craniotomy can vary depending on the complexity of the surgery but often includes time in hospital followed by rehabilitation and ongoing monitoring.
Adjusting to life after surgery
David was warned that during his recovery, he might become “childlike” in his thinking. He describes losing half his savings due to impaired cognitive ability in the months after surgery, which he feels could have been avoided with better access to long-term post-operative support. He also had kidney failure during surgery, requiring ongoing blood tests.
“Six months after surgery, I started to regain executive function. That was the turning point.”
During this time, David moved from London to Port Sunlight on the Wirral in search of a quieter life and recovery.
Career disruption and rebuilding
David worked with IBM across Europe for 40 years and briefly for the Civil Service. However, IBM let him go following a resourcing reorganisation. He made a legal claim for what he believed was an unfair dismissal and eventually started over.
“I even got a new job as National Business Events Manager in the Civil Service. Unfortunately, that role ended due to recent Government cutbacks.”
Living with seizures and ongoing challenges

Despite his improvements, David continued to live with seizures caused by scarring left over by the tumour. One such seizure even caused him to fall down the stairs. He takes regular medication and remains under the care of neurologists — though accessing timely scans has been difficult.
Still, he’s hopeful things will improve. He has appointments coming up, though he notes that without recent scans, there’s only so much that can be done.
Looking ahead with gratitude
David is no longer in the hospital. Although his fatigue lingers, he says he feels “greatly improved,” having not had a seizure in some time. And he’s not done yet.
“Despite everything, I still want to contribute. I’m creative, I’m resilient, and I’ve got more to give.”
His experience of surviving the largest meningioma ever seen at St George’s Hospital, enduring a life-changing surgery, losing income, and rebuilding — all while adjusting to a new way of life — is a powerful reminder of what can be overcome.
Final thoughts
David hopes his story raises awareness about the need for early diagnosis, proper post-surgery support, and the value of continued neurological care.
“I was lucky. I had a choice — and I’m still here. I want people to know that you can rebuild your life after something like this. You’re not alone.”
Category: News
Published: 20 June 2025